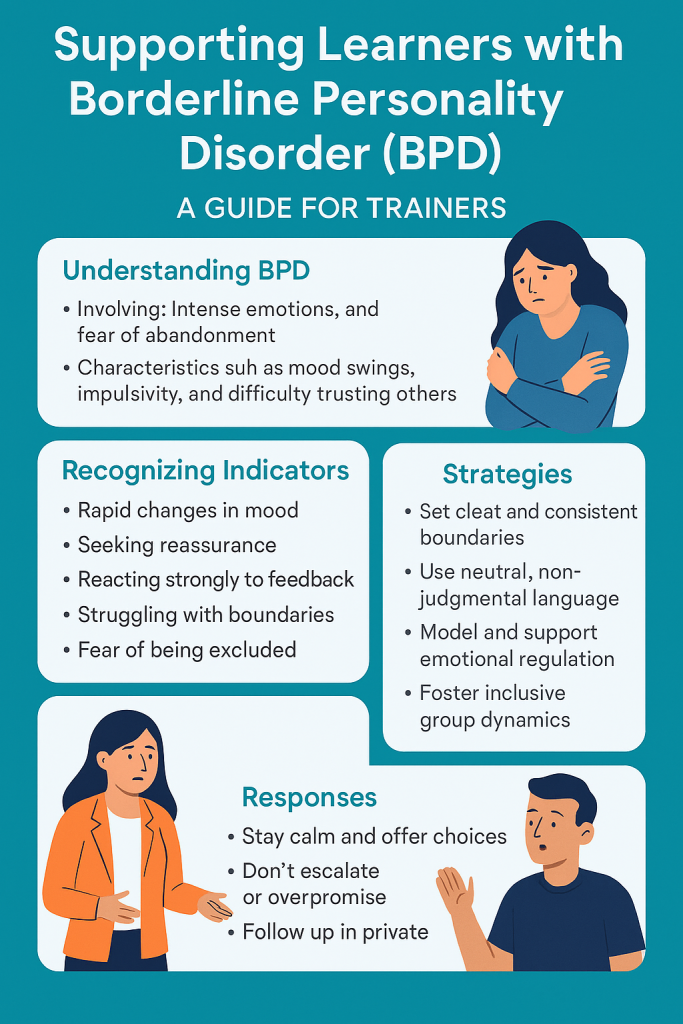
Borderline Personality Disorder (BPD) is a complex mental health condition characterised by intense emotional experiences, unstable interpersonal relationships, fear of abandonment, and difficulties with self-image and impulse control (NHS, 2023). For professional trainers, awareness of BPD is essential to creating psychologically safe learning environments that support emotional regulation, minimise misinterpretation, and empower learners. This guide outlines the key features of BPD, practical strategies for training delivery, and professional boundaries required to support learners effectively.
1. Understanding Borderline Personality Disorder in the Training Context
BPD affects approximately 1–2% of the population and often stems from early trauma, invalidation, or attachment disruptions (Linehan, 1993). It is not a choice or attitude issue—it is a deeply rooted emotional regulation disorder.
Key features include:
Fear of abandonment or rejection
Rapid shifts in mood and self-identity
Intense or unstable relationships
Difficulty trusting others
Impulsivity or self-destructive behaviours
Why it matters: A delegate with BPD may be highly engaged one moment and withdrawn or upset the next. They may also misinterpret neutral feedback as personal rejection. These behaviours can disrupt learning if misunderstood or mishandled (National Institute for Health and Care Excellence [NICE], 2009).
2. Recognising Potential Signs of BPD in Training
As a trainer, you are not expected to diagnose. However, being trauma- and personality-aware means noticing patterns and adjusting your practice accordingly.
Possible behavioural indicators:
Fluctuating engagement (over-involvement followed by withdrawal)
Intense reactions to perceived slights or group dynamics
Seeking excessive reassurance
Sudden changes in mood or expressions of self-doubt
Struggles with boundaries, e.g., over-disclosure
Example: A learner reacts strongly to being asked to switch groups, perceiving it as exclusion. A sensitive trainer recognises this as emotional dysregulation, not defiance or disrespect.
3. Strategies to Support Learners with BPD
Creating a stable, empathetic, and clearly bounded learning environment is key to supporting learners with BPD traits or diagnoses.
a. Set Clear and Consistent Boundaries
Predictable boundaries create a sense of emotional safety.
Example: Establish ground rules at the start: “All feedback in this course is about the work, not the person. Everyone is learning.”
Why: Prevents misinterpretation and reduces fear of abandonment (Gunderson et al., 2018).
b. Use Emotionally Neutral, Non-Judgmental Language
Avoid dramatic language, sarcasm, or vague comments that may be misread.
Example: Instead of saying, “That presentation was a bit of a disaster,” try: “Let’s work on clarity and structure for next time.”
Why: People with BPD are often hypersensitive to tone and ambiguity (Lieb et al., 2004).
c. Model and Support Emotional Regulation
Create opportunities for learners to pause, reflect, and regulate.
Example: Offer regular breaks, and build in reflection points. “Let’s take 3 minutes to reflect quietly before moving on.”
Why: Supports self-regulation and helps learners avoid emotional overwhelm (Linehan, 1993).
d. Foster Inclusive Group Dynamics
Group-based activities can trigger feelings of rejection or comparison.
Example: Use structured roles during group tasks to prevent feelings of exclusion. Rotate roles to ensure balanced participation.
Why: Encourages equitable engagement and prevents social stressors that may escalate emotional reactivity.
4. Responding Supportively to Emotional Outbursts or Disruption
Trainers may occasionally face emotional intensity from a delegate with BPD. Responses should be calm, empathetic, and boundaried.
Do:
Remain calm and grounded
Acknowledge feelings without over-personalising: “It sounds like you’re feeling frustrated. Let’s talk after the session.”
Offer choices (e.g., step out, take a break, reschedule)
Don’t:
Argue, challenge, or match emotional intensity
Publicly address the issue unless necessary
Make promises you cannot keep
Example: A learner says, “Everyone hates me here.”
Trainer response: “It’s okay to feel that way sometimes. Let’s talk more privately after the session. You’re not alone.”
Why: This response validates emotion without escalating the situation or reinforcing the belief (MHFA England, 2023).
5. Embedding Support Structures in Training
Tool/Technique Description Why It Works
Private Check-Ins Short one-to-one conversations at key stages Builds trust and allows emotional venting in a controlled space
Structured Feedback Templates Clear, factual, and strengths-based Reduces personalisation of constructive feedback
Group Agreements Created collaboratively at the start Promotes shared responsibility for safety and respect
Trauma-Informed Practice Acknowledge that behaviours may be adaptations Prevents pathologising or blaming
6. Trainer Boundaries and Self-Care
Supporting a learner with BPD traits requires empathy and strong boundaries.
Guidelines:
Stay professional. Be warm but not overly involved.
Avoid over-accommodation. Fairness and consistency help everyone.
Don’t offer therapy. Refer concerns to relevant support (e.g., wellbeing services, MHFA, HR).
Reflection prompt: Am I trying to “rescue” this learner? How can I support without over-functioning?
7. Reviewing and Adapting the Learning Environment
Include mental health considerations in your course evaluations:
Sample questions:
“Did the trainer maintain a respectful and consistent environment?”
“Were you supported when you felt overwhelmed or unsure?”
“Did group work feel safe and inclusive?”
Use qualitative feedback to identify emotional triggers in the training structure and adjust accordingly.
Conclusion
Supporting learners with Borderline Personality Disorder traits is not about managing “difficult behaviour” but about understanding emotional vulnerability and promoting safety, clarity, and empathy. With the right awareness and structure, trainers can unlock engagement and reduce conflict—helping every learner grow.
References (Harvard Style)
Gunderson, J.G., et al., 2018. Borderline Personality Disorder: A Clinical Guide, 3rd ed. Washington DC: American Psychiatric Publishing.
Lieb, K., Zanarini, M.C., Schmahl, C., Linehan, M.M. and Bohus, M., 2004. Borderline personality disorder. The Lancet, 364(9432), pp.453-461.
Linehan, M.M., 1993. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press.
MHFA England, 2023. Mental Health First Aid: Personality Disorders. [online] Available at: https://www.mhfaengland.org [Accessed 7 June 2025].
National Institute for Health and Care Excellence (NICE), 2009. Borderline personality disorder: recognition and management. [CG78] [online] Available at: https://www.nice.org.uk/guidance/cg78 [Accessed 7 June 2025].
NHS, 2023. Borderline personality disorder (BPD). [online] Available at: https://www.nhs.uk/mental-health/conditions/borderline-personality-disorder/ [Accessed 7 June 2025].
Practical Guide for Trainers: Borderline Personality Disorder (BPD) Awareness in Training Environments